|
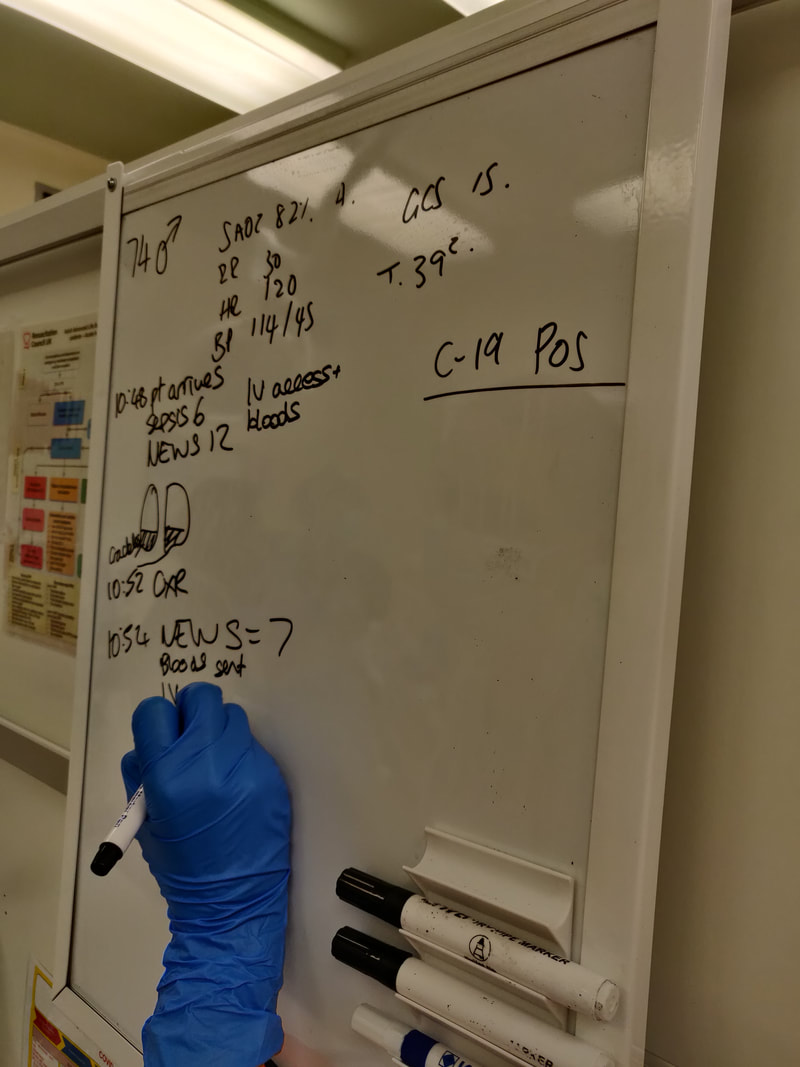
This sim focussed on a life threatening presentation of a patient with end-stage renal disease (ESRD). Thanks to Suzy Connor and Andy Connor for their help with this simulation and information for this blog. The simulated case: A man in his 60s who has haemodialysis on Monday-Wednesday-Friday, presented on a Monday morning (see Fig 1 here) with shortness of breath and fatigue. Investigations revealed pulmonary oedema with hyperkalaemia and anaemia. Their case was discussed with the renal consultant on-call and they were transferred for dialysis. Afterwards we reviewed management of a major AV fistula bleed. What did we think? In debrief we discussed: Pulmonary oedema: Think about what questions you would ask the patient in these circumstances. Important renal points are (n.b. the patient’s “dry weight” is the estimated number of kilograms they aim to weigh following a dialysis session):
Other than this, it could be that their dry weight estimate is off e.g. they have lost muscle and fat mass without adjustment of their dry weight so now the body is made up of a higher proportion of water. If we are considering that a cardiac insult has caused the pulmonary oedema, the troponin result may be helpful if very high or much higher than previous. But obviously could be high from ESRD, so rely more on the ECG and history. Renal disease also puts the patient at risk of uraemic pericarditis which could cause the pulmonary oedema. In terms of treatments, loop diuretics are unlikely to help even if the patient produces urine as they often don't increase the output. A GTN infusion might help as a holding measure, but the definitive treatment is dialysis. Hyperkalaemia: Our hyperkalaemia protocol is found on the G:/ drive. It has a specific stream for fluid overloaded patients with the dextrose given at a higher concentration. Insulin and dextrose will work as a holding measure pending urgent dialysis. IV sodium bicarbonate may worsen fluid overload. Venepuncture and analgesia in ESRD: This patient has an arteriovenous fistula for dialysis and this is clearly very important for their survival. Avoid the fistula arm (which most likely will be on their non-dominant side) when taking blood, and go as distal as possible. Also avoid BP cuffs on the fistula side. Consider this too when taking blood from a patient who may require dialysis in the future and may therefore may need a AV fistula creating - go dominant side and as distal as feasible. If the attempt fails, escalate early rather than continue attempts. Pain relief can be tricky when renal function is poor. Generally the plan is to avoid opiates, although if necessary can use immediate-release low dose oxycodone. Avoid NSAIDs unless the patient has no urine output - in this case NSAIDs can actually be used as there is no renal function left to preserve. Who to escalate to? There is always at least one renal physician on-call 24/7: switchboard will advise who is first-on-call. We discussed that in this case it could be that ITU is needed due to the level of organ dysfunction. Bleeding AV fistula: For a dialysis patient, their fistula is their lifeline. Fistula problems can easily be life-threatening - have a really low threshold for admission. KidneyCareUK state: “Scabs at needling sites that are raised, enlarging bumps (aneurysms) along the access, shiny skin over the vascular access and/or loss of skin pigment over an aneurysm all require urgent review and, if left untreated, could potentially lead to a life-threatening bleed”.
To do:
There is a renal guidelines booklet on EDIS [ ] CAT tourniquet refresher video [ ] Consider the additional questions you might now ask a patient receiving dialysis when they present to the ED [ ] If you took part in the sim, you can use this blog as a starter to reflect on your own experience of it [ ] Blog by: James Keitley - ED sim fellow - on behalf of the ED sim team. --------------- For clinical decisions please refer directly to primary sources. This blog may not be updated. All images copyright- and attribution-free in the public domain or taken by the author.
0 Comments
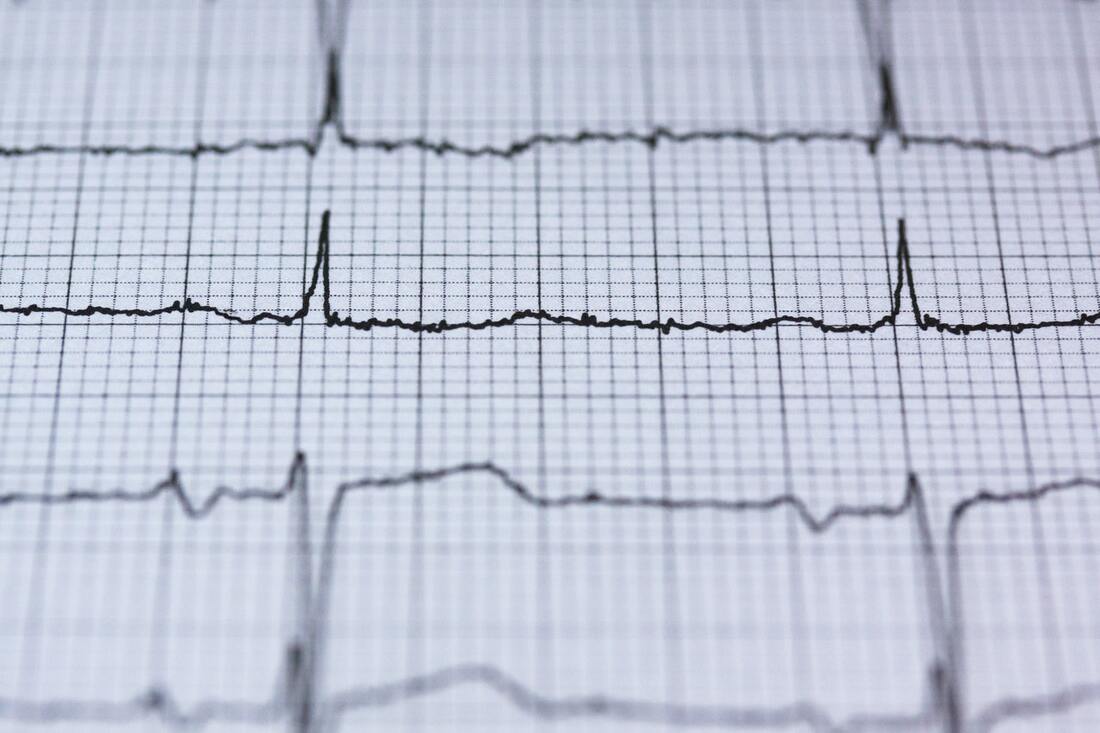
This week we covered two scenarios, TCA overdose and a near-fatal asthma exacerbation. This blog will cover TCA overdose. Click the links to view previous blogs on paediatric and adult asthma. We’ve simulated TCA overdose earlier this year too but didn’t blog at the time, so here is a reflection of the scenario. Thanks to Annette and Laura for planning and running this sim. The simulated case: A teenage patient presents having taken an overdose of a tricyclic antidepressant, agitated and combative. What happened? The simulated patient was pre-alerted and team roles were assigned. Due to agitation, their initial assessment and treatment was challenging. They were given IM ketamine to facilitate assessment - this was “procedural sedation”, ideally with the preparation of gaining observations, IV access and ECG; not possible in the combative child/adolescent. Later they had several seizures. They were given IV sodium bicarbonate to counteract the cardiotoxic effect of amitriptyline. What did we think? In debrief we discussed: Danger of TCA overdose: The toxic dose is relatively low (see table on TOXBASE for different medications), so take it seriously. The concerning features are:
Anticholinergic syndrome could be recognised (tachycardia, mydriasis, dry mouth) and some TCAs can also contribute to serotonin syndrome. Bicarbonate:
We discussed how one of the central actions of TCAs on the heart is through blockade of sodium channels. The key management - sodium bicarbonate - may act through several mechanisms to interfere with this. TOXBASE has a helpful table of doses, but the bottom line if there are ECG changes, start the bicarbonate and titrate it according to the ECG. In cardiac arrest the adult dose is a rapid bolus of 100 mmol (i.e.100 mL 8.4%) sodium bicarbonate, or of 2-4 mL/kg of 4.2% if given peripherally in a child. If you only have a different concentration of bicarbonate, you can alter the amount to still give 100mmol (table on TOXBASE). 8.4% - 100mL 4.2% - 200mL 1.4% - 600mL 1.26% - 667mL It’s a really irritant drug to give, so ideally get a large vein and give a large flush following it, but it can be given into an intraosseous line as long as the line is flushed before administering other time critical medications. Note that in this case, amiodarone should be avoided as it can additionally extend the QT interval. It is also a situation where CPR may need to continue for several hours. Seizures: If not self-limiting, then IV benzodiazepines can be given. Seizures may be a sign that intubation and ventilation is required, although any drop in GCS below 13 should get you considering this or a rapid change in neurological status. Don’t wait for the seizure! Controlling the situation: This patient received IM ketamine. For pharmacological options, TOXBASE suggests oral, IV or IM benzodiazepines, IM haloperidol or ketamine. To do: Explore LITFL for ECGs in the case of tricyclic antidepressant overdose here [ ] Overview of toxicity here, or an EMJ review here [ ] If you took part in the sim, you can use this blog as a starter to reflect on your own experience of it [ ] Blog by: James Keitley and Annette Rickard on behalf of the ED sim team. --------------- For clinical decisions please refer directly to primary sources. This blog may not be updated. All images copyright- and attribution-free in the public domain or taken by the author. Recently we’ve run a few simulations where the participants cannot speak out loud and must focus on nonverbal communications, based on the EM3 plan. The original intention of the simulation is to hone skills that are helpful when our verbal communications are hampered by red PPE.
What did we think?
In debrief we discussed: The role of quiet: Silence in resus has its advantages. Distractions were minimal. It forced the closing of loops where people confirmed tasks had been received. And the team leader at the head of the bed in the amber zone was receptive to communications coming towards them. Reflect on any noisy patient encounters you have had and their effect on your stress, communication or decision-making. Perhaps noise was unavoidable in that situation, or perhaps it was greater than necessary. Part of the mitigation of this is systematic - how we design hospitals, monitors, room shapes, materials, doors, use of space and so on. But part we can influence, or at least be aware of when it is starting to impair processes so it can be highlighted. Two sides of the communication coin: Every time we receive verbal communication from a colleague it comes packaged with non-verbal cues e.g. posture, facial expression, eye contact or lack of, potentially written word and so on. These adjust the message received and can alter it drastically. They can reinforce what we are saying, or if incongruent they can confuse or completely change the message. So it is critical that our verbal and non-verbal sides are in-keeping with each other. When we wear red PPE we are reducing clarity of voice, availability of facial expressions, eye contact and more, and therefore putting ourselves at higher risk of being misunderstood. Clearly any hearing impairment of involved staff or patients is going to make this more challenging. As a baseline the understanding of a message is weighted towards the non-verbal cues, so now these are even more critical. Think about a time you have had a misunderstanding at work and which factors contributed to it. Perhaps it was a misunderstanding over email where we are stripped down to simply written word only, or on the phone with spoken word only. Perhaps HALT factors were involved and affected how the message was communicated. Perhaps there was confusion over who was to act on a spoken instruction because of a lack of direction or non-verbal back-up. Personally I can think of recent examples of all of these, they happen commonly. What can we do about these situations? We can ensure we specifically think about the power our non-verbal communication has.
These are just a couple of examples, have a think about specifics in your role. Awareness of others: It was pointed out during this sim that there is a risk of losing awareness of what others are doing within the team and focussing solely on your own task if there is no verbal communication. This highlights the fact that the ideal is to have both clear verbal and nonverbal aspects, including team mini-summaries to ensure everyone is on the same page and sharing the same mental model. To do: Think about a recent misunderstanding or a communication challenge and reflect on how you would change what happened next time [ ] NursingTimes article on nonverbal communication [ ] If you took part in the sim, you can use this blog as a starter to reflect on your own experience of it [ ] Blog by: James Keitley - ED sim fellow - on behalf of the ED sim team. --------------- For clinical decisions please refer directly to primary sources. This blog may not be updated. All images copyright- and attribution-free in the public domain or taken by the author. |
Categories
All
The Derrifoam BlogWelcome to the Derrifoam blog - interesting pictures, numbers, pitfalls and learning points from the last few weeks. Qualityish CPD made quick and easy..... Archives
October 2022
|