|
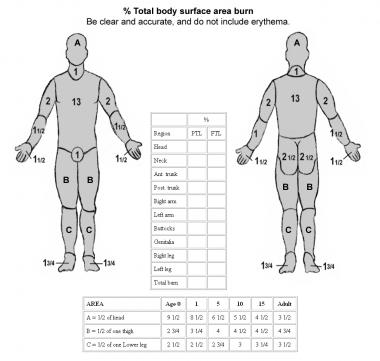
Baxter (parkland) formula: 2-4ml/kg x body weight x %burn
Beware fluid creep: just because fluids are good in burns, does not necessarily mean more fluids are better. Consider starting at lower end of 2-4 ml/kg Excess fluids cause: burn progression, non-wound oedema, compartment syndromes, impaired gas exchange, cerebral oedema Remember that fluids are COLD, warm them before infusing. Clare Bosanko, Febr 2017
6 Comments
AirwaySigns: reduced level of consciousness, voice change, perioral or perinasal burns (not just facial burns), soot in the oropharynx (not just nose), erythema or oedema of tongue, stridor Undertaking intubation:
Pitfalls:
Clare Bosanko, Febr 2017
ED Approach to a major paediatric burn
Assessment
Management (consultant led care)
The suggested minimum threshold for referral into specialised burn care services can be summarised as:
If burn wound changes in appearance / signs of infection or there are concerns regarding healing then discuss with a specialised burn service. If there is any suspicion of Toxic shock syndrome (TSS) then refer early. Click here for full guideline: http://www.britishburnassociation.org/ Clare Bosanko, Jan 2017 Link to previous learning blog: http://derriforded.weebly.com/derrifoam-blog/gems-wdwlt
First aid Stop the burning process: remove clothing, don’t remove if adherent Cool with running water, for 20 minutes Temporary dressing: cling film Elevate limbs Basic principles
How are hospitals that look after burned patients organised? Facility > unit > centre (National Burn Care Referral Guidance)
In the South West: Derriford is a burns facility. Bristol Southmead is a burns unit for adults Morriston, Swansea is a burns centre for adults Bristol Children’s Hospital is burns centre for children C Bosanko; Jan 2017
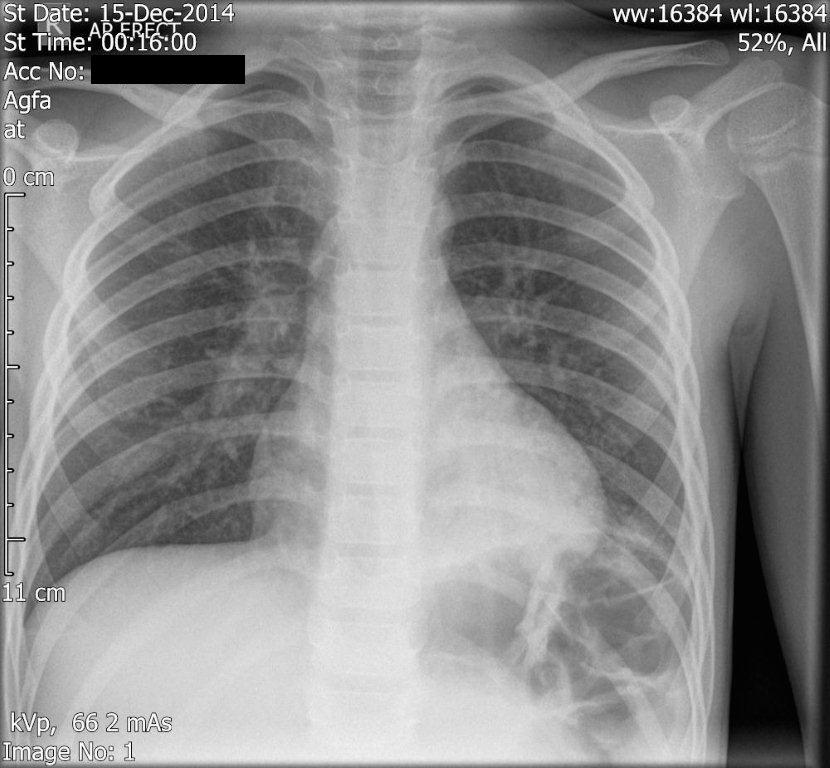
by Adam Herbstritt6 year old presents unwell, febrile, viral, coryzal with some focal chest signs.
This Xray was performed in ED - what do you see? |
Categories
All
The Derrifoam BlogWelcome to the Derrifoam blog - interesting pictures, numbers, pitfalls and learning points from the last few weeks. Qualityish CPD made quick and easy..... Archives
October 2022
|