|
Continuing the surgical theme today we simulated a young patient with a perforated appendix. Next week's SimFridays is cancelled for Christmas. Hope everyone is able to relax and spend some time with family or friends - even if that might now be in virtual form. Next month the plan is for a mental health theme - if anyone has ideas of how best to approach simulation in this month please get in touch. The simulated case: A 19 year old woman presented with abdominal pain during the night, and due to ED pressures she had been waiting to be assessed in majors at the time of morning handover. What happened? The ED team assessment in majors found her to be tachycardic and tachypnoeic, with uncontrolled pain. She had an A-E assessment followed by management of pain, fluid resuscitation and antibiotics - then the potential causes of this presentation were considered. What did we think? In debrief we discussed: Imaging: We talked about the considerations of using CT in this patient group. Generally, ultrasonography is preferred in young women due to the higher incidence of gynaecological cause and the radiation involved in CT. However, as discussed in the simulation, the timing of the imaging must also be considered - if there is going to be a long delay for USS then the preference might shift to CT. If there is a high suspicion of appendicitis with shock, then immediate appendicectomy may be performed however if there is diagnostic uncertainty then there is value in imaging, and the evidence suggests this does not cause additional delay in general. (ASGBI commissioning guide 2014, see p12-13). Gynaecological vs general surgical causes:
This patient was shocked and had an empty bladder scan, therefore a urine pregnancy test had not been possible. We talked about while there is diagnostic uncertainty it may be reasonable to involve both teams. β-HCG can be added-on to blood already taken. Simultaneous treatments: In this case there were competing demands on our colleagues time and resources. There were paracetamol, antibiotics, fluid, and analgesia to give - and only one cannula - and there was also discussion to be had with ED seniors, radiology (+/- scan requesting), and the surgical team. Managing these priorities was a key part of the thinking in this scenario. What would be your strategy in this circumstance be? Overnight delays: We talked about how after the initial front-door assessment there can be delays in being seen definitively, and patients have the potential to worsen during this time. The expected benefit from having a greater number of nursing colleagues is a repeated theme from SimFridays feedback, and today this was also discussed as something that would benefit patients like these. Other feedback included having patients like this allocated to the more visible bays, or if in the corridor then under the care of an assigned nurse. In this simulated case the patient went on to have a CT abdomen which showed acute appendicitis with perforation, and they went to theatre. To do: The next time you have multiple tasks to complete, take a moment to think through your thought processes. You might instinctively know which tasks take highest priority - analyse why you know this to be the case, what would change your mind, when is this not the case etc [ ] If you took part in the sim, you can use this blog as a starter to reflect on your own experience of it [ ] Blog by: James Keitley ED sim fellow --------------- For clinical decisions please refer directly to the guidance. This blog may not be updated. All images copyright- and attribution-free in the public domain or taken by the author.
0 Comments
I have been reflecting on my workplace experiences over the last few months and how I think I am responding to our pressured and uncertain world and how that relates to my relationships with colleagues and what I observe in those beside me. From time to time I have noticed that my response to feedback will be defensive, and I suspect that others respond in a similar way. Whilst understandable it has consequences in my clinical practice, how the care is delivered by the team and how that is received by the patient. At first there may be blame and criticism leading to datix report and complaints. This leads to conflict, defensiveness and eventually to individual disengagement. I know this because I have experienced this and have disengaged from time to time; it is my way of coping, and I am conscious that others might be doing that too. I personally start to lose the sense of joy and the importance of the work that we do, the difference we make in such an important moment in a patient’s life.  We need to embrace a compassionate and grown up approach to sustain a high performing team. It’s important to create psychological safety and trust; to ask ourselves what would it be like if we could share difference and see it as enrichment of our clinical practice, counterviews are appreciated for what they are as different; and if there is concern about the safety and quality of that approach it is highlighted generously with the motivation to help and educate. From our own and colleagues’ experiences, it can be quite disheartening to face any kind of criticism from peers or managers. There is some kind of fear that one is being blamed for mistakes, which tends to happen more often in a high risk, pressured situation when our calmness and generosity is more in need. We are lucky to have a No Blame Policy at UHP but still why do we always feel guilty when we have taken action in the best interests of a patient at the time, then later, it is proven not to have been the right thing to do? Perhaps we need to adopt alternative ways to approach these incidents. Use them as a case study at meetings or handovers to avoid similar issues again… Human to human communication may reflect a much better outcome and resolve any misunderstandings amongst colleagues. No-one should be made to feel that they are being punished for having genuinely tried to act in the best interests of their patient, but there may be some learning that comes from this. I recently read this concept somewhere and perhaps if we can all use similar thoughts, we can have a better understanding and be supportive, caring and compassionate towards each other. This is not any different to us wanting to treat our patients the way we would like to be treated, only this time we are thinking about looking after us, after each other. By this we will clap for ourselves as we will be heroes for each other. Each time you have to challenge someone please remember the following: 1)This person has beliefs, perspectives, and opinions, just like me. 2)This person has hopes, anxieties, and vulnerabilities, just like me. 3)This person has friends, family, and perhaps children who love them, just like me. 4)This person wants to feel respected, appreciated, and competent, just like me. 5)This person wishes for peace, joy, and happiness, just like me. We are living in a very unprecedented and challenging world. Let’s care, be kind and be fair. We are the best team but we can now move towards perfection by “being the change we want to see in the Team”. AuthorWritten by Shadna Lallchand, ENP, Derriford ED December 2020 Today we looked at how we investigate older people with traumatic injury. The TARN report on major injury in older people (2017) showed differences in how these patients are looked after compared to younger trauma patients. A high number of injuries occur from falls from standing height in the home, and major injuries can be difficult to identify. In related news, over the next couple of months we will simulate some trauma calls to run through processes and identify any potential system errors when caring for trauma patients in the emergency department. The simulated case: A 90 year old female who had been found on the floor of her lounge by carers. She has been unable to describe the day’s events but has pain in her hip.
What did we think? In debrief we discussed: Imaging: We talked about the chest examination involving a firm palpation around the sides and back of the chest if possible, to ensure we don’t miss injury around the sides of the patient. In this patient, with definite head and hip injuries on opposite sides of the body, with low saturations and pain around the side of the chest there are indications for a CT trauma scan to look for underlying injury. In other cases it may be entirely appropriate to have a CT head and a hip x-ray. Each case should be considered and discussed with someone experienced in seeing such patients.
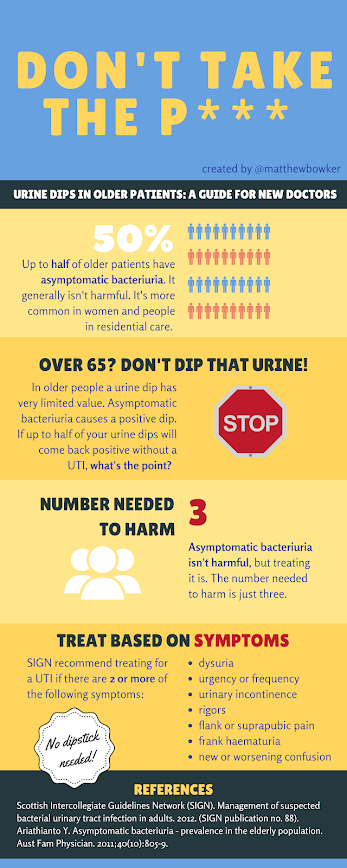
We hear older patients say they have recurrent urinary infections - and this may of course still be the case - but consider whether there is something else that is being misdiagnosed based on positive urine dip/culture. Start afresh. This is only about leukocytes/nitrites and infection, so if you’re using the urine dip for another purpose this doesn't apply! Physiological considerations: We talked about how particularly in older people it needs to be considered whether their past medical history, frailty or medication history might be affecting the clinical picture and lead to error. For instance are they taking a medication to control heart rate that affects a tachycardic response to bleeding? By definition frailty is a reduced ability to keep homeostasis after insult, so normal observations may not be reassuring, and may represent a lack of response to injury where there should be a response. To do: RCEM learning on silver trauma [ ] Have a look at the GP guidance on UTI in those over 65 years of age [ ] If you took part in the sim, you can use this blog as a starter to reflect on your own experience of it [ ] Blog by: James Keitley ED sim fellow --------------- For clinical decisions please refer directly to the guidance. This blog may not be updated. All images not cited are copyright- and attribution-free in the public domain or taken by the author. |
Categories
All
The Derrifoam BlogWelcome to the Derrifoam blog - interesting pictures, numbers, pitfalls and learning points from the last few weeks. Qualityish CPD made quick and easy..... Archives
October 2022
|