|
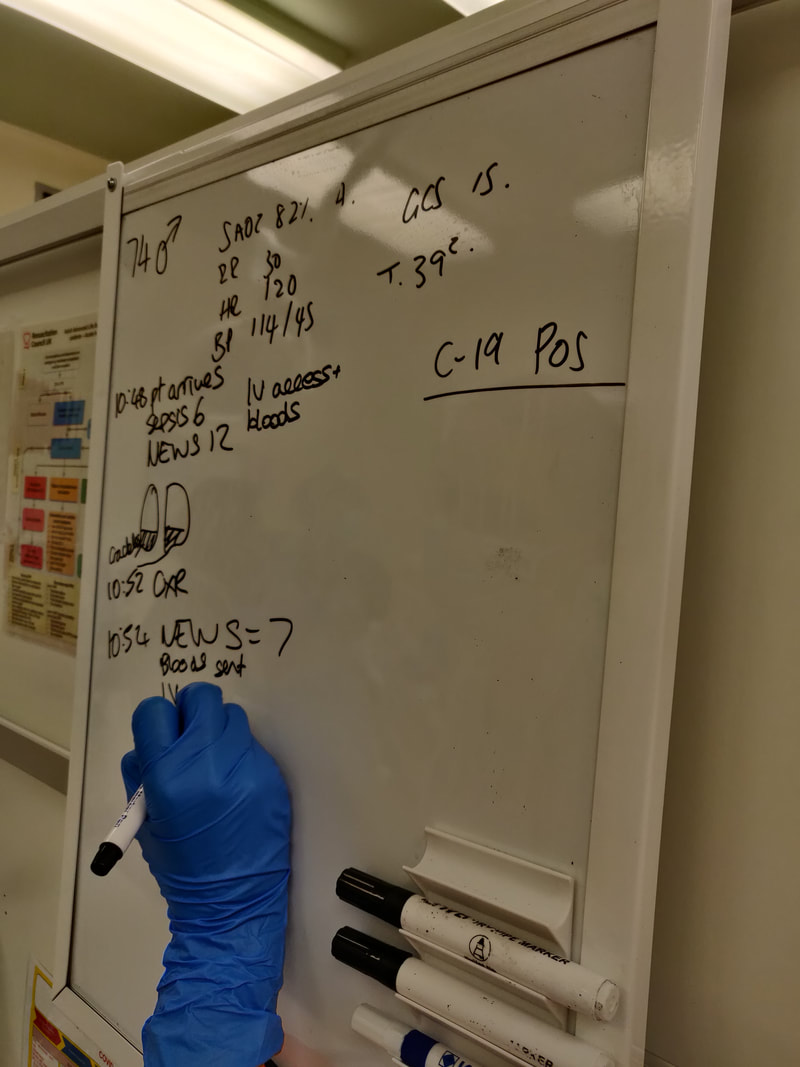
Recently we’ve run a few simulations where the participants cannot speak out loud and must focus on nonverbal communications, based on the EM3 plan. The original intention of the simulation is to hone skills that are helpful when our verbal communications are hampered by red PPE.
What did we think?
In debrief we discussed: The role of quiet: Silence in resus has its advantages. Distractions were minimal. It forced the closing of loops where people confirmed tasks had been received. And the team leader at the head of the bed in the amber zone was receptive to communications coming towards them. Reflect on any noisy patient encounters you have had and their effect on your stress, communication or decision-making. Perhaps noise was unavoidable in that situation, or perhaps it was greater than necessary. Part of the mitigation of this is systematic - how we design hospitals, monitors, room shapes, materials, doors, use of space and so on. But part we can influence, or at least be aware of when it is starting to impair processes so it can be highlighted. Two sides of the communication coin: Every time we receive verbal communication from a colleague it comes packaged with non-verbal cues e.g. posture, facial expression, eye contact or lack of, potentially written word and so on. These adjust the message received and can alter it drastically. They can reinforce what we are saying, or if incongruent they can confuse or completely change the message. So it is critical that our verbal and non-verbal sides are in-keeping with each other. When we wear red PPE we are reducing clarity of voice, availability of facial expressions, eye contact and more, and therefore putting ourselves at higher risk of being misunderstood. Clearly any hearing impairment of involved staff or patients is going to make this more challenging. As a baseline the understanding of a message is weighted towards the non-verbal cues, so now these are even more critical. Think about a time you have had a misunderstanding at work and which factors contributed to it. Perhaps it was a misunderstanding over email where we are stripped down to simply written word only, or on the phone with spoken word only. Perhaps HALT factors were involved and affected how the message was communicated. Perhaps there was confusion over who was to act on a spoken instruction because of a lack of direction or non-verbal back-up. Personally I can think of recent examples of all of these, they happen commonly. What can we do about these situations? We can ensure we specifically think about the power our non-verbal communication has.
These are just a couple of examples, have a think about specifics in your role. Awareness of others: It was pointed out during this sim that there is a risk of losing awareness of what others are doing within the team and focussing solely on your own task if there is no verbal communication. This highlights the fact that the ideal is to have both clear verbal and nonverbal aspects, including team mini-summaries to ensure everyone is on the same page and sharing the same mental model. To do: Think about a recent misunderstanding or a communication challenge and reflect on how you would change what happened next time [ ] NursingTimes article on nonverbal communication [ ] If you took part in the sim, you can use this blog as a starter to reflect on your own experience of it [ ] Blog by: James Keitley - ED sim fellow - on behalf of the ED sim team. --------------- For clinical decisions please refer directly to primary sources. This blog may not be updated. All images copyright- and attribution-free in the public domain or taken by the author.
0 Comments
Leave a Reply. |
Categories
All
The Derrifoam BlogWelcome to the Derrifoam blog - interesting pictures, numbers, pitfalls and learning points from the last few weeks. Qualityish CPD made quick and easy..... Archives
October 2022
|