|
This week we covered two scenarios, TCA overdose and a near-fatal asthma exacerbation. This blog will cover TCA overdose. Click the links to view previous blogs on paediatric and adult asthma. We’ve simulated TCA overdose earlier this year too but didn’t blog at the time, so here is a reflection of the scenario. Thanks to Annette and Laura for planning and running this sim. The simulated case: A teenage patient presents having taken an overdose of a tricyclic antidepressant, agitated and combative. What happened? The simulated patient was pre-alerted and team roles were assigned. Due to agitation, their initial assessment and treatment was challenging. They were given IM ketamine to facilitate assessment - this was “procedural sedation”, ideally with the preparation of gaining observations, IV access and ECG; not possible in the combative child/adolescent. Later they had several seizures. They were given IV sodium bicarbonate to counteract the cardiotoxic effect of amitriptyline. What did we think? In debrief we discussed: Danger of TCA overdose: The toxic dose is relatively low (see table on TOXBASE for different medications), so take it seriously. The concerning features are:
Anticholinergic syndrome could be recognised (tachycardia, mydriasis, dry mouth) and some TCAs can also contribute to serotonin syndrome. Bicarbonate:
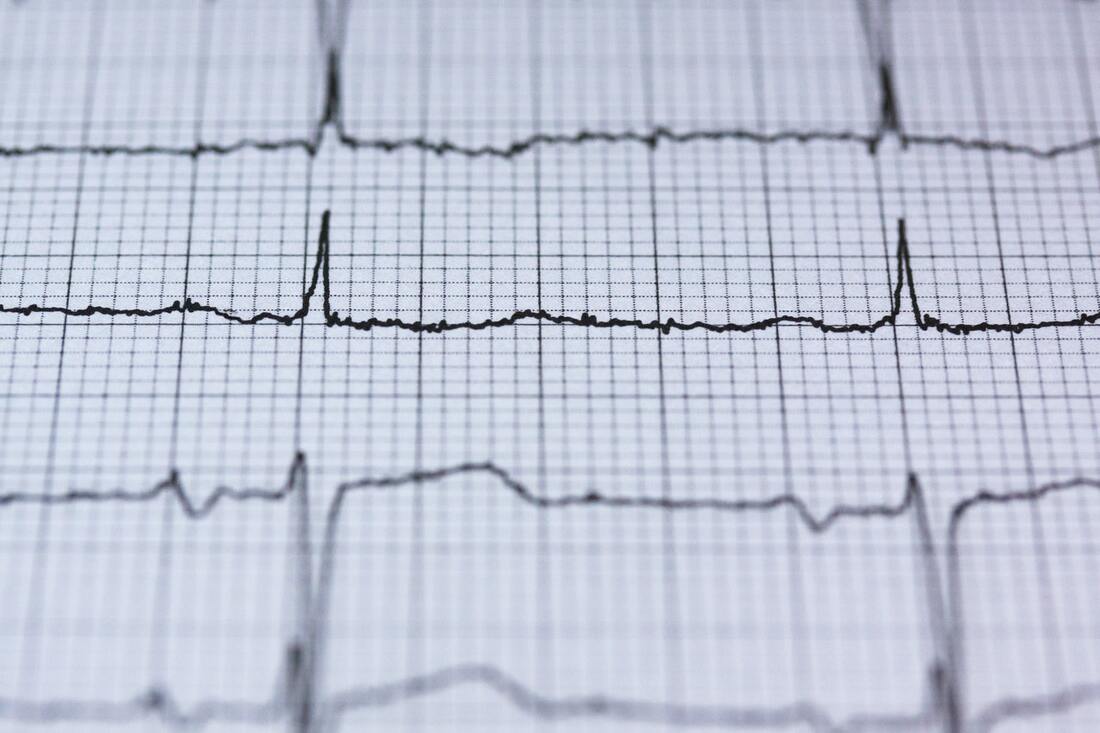
We discussed how one of the central actions of TCAs on the heart is through blockade of sodium channels. The key management - sodium bicarbonate - may act through several mechanisms to interfere with this. TOXBASE has a helpful table of doses, but the bottom line if there are ECG changes, start the bicarbonate and titrate it according to the ECG. In cardiac arrest the adult dose is a rapid bolus of 100 mmol (i.e.100 mL 8.4%) sodium bicarbonate, or of 2-4 mL/kg of 4.2% if given peripherally in a child. If you only have a different concentration of bicarbonate, you can alter the amount to still give 100mmol (table on TOXBASE). 8.4% - 100mL 4.2% - 200mL 1.4% - 600mL 1.26% - 667mL It’s a really irritant drug to give, so ideally get a large vein and give a large flush following it, but it can be given into an intraosseous line as long as the line is flushed before administering other time critical medications. Note that in this case, amiodarone should be avoided as it can additionally extend the QT interval. It is also a situation where CPR may need to continue for several hours. Seizures: If not self-limiting, then IV benzodiazepines can be given. Seizures may be a sign that intubation and ventilation is required, although any drop in GCS below 13 should get you considering this or a rapid change in neurological status. Don’t wait for the seizure! Controlling the situation: This patient received IM ketamine. For pharmacological options, TOXBASE suggests oral, IV or IM benzodiazepines, IM haloperidol or ketamine. To do: Explore LITFL for ECGs in the case of tricyclic antidepressant overdose here [ ] Overview of toxicity here, or an EMJ review here [ ] If you took part in the sim, you can use this blog as a starter to reflect on your own experience of it [ ] Blog by: James Keitley and Annette Rickard on behalf of the ED sim team. --------------- For clinical decisions please refer directly to primary sources. This blog may not be updated. All images copyright- and attribution-free in the public domain or taken by the author.
0 Comments
Leave a Reply. |
Categories
All
The Derrifoam BlogWelcome to the Derrifoam blog - interesting pictures, numbers, pitfalls and learning points from the last few weeks. Qualityish CPD made quick and easy..... Archives
October 2022
|