|
For our first month of SimFridays we’re looking at paediatrics, and if you couldn’t join us for the first session (4th September) this blog covers some of the learning points. We will be aiming to run simulations every Friday at 11am - go to derriforded.com/sim particularly if you have suggestions of what we should cover! The simulated case: Dylan is a 6 year old child brought in by his mother. He was short of breath and wheezy at school, and his inhaler didn’t seem to resolve it. What would you do? How would you feel approaching Dylan?
What did we think? We talked through the scenario in debrief. Key points were:
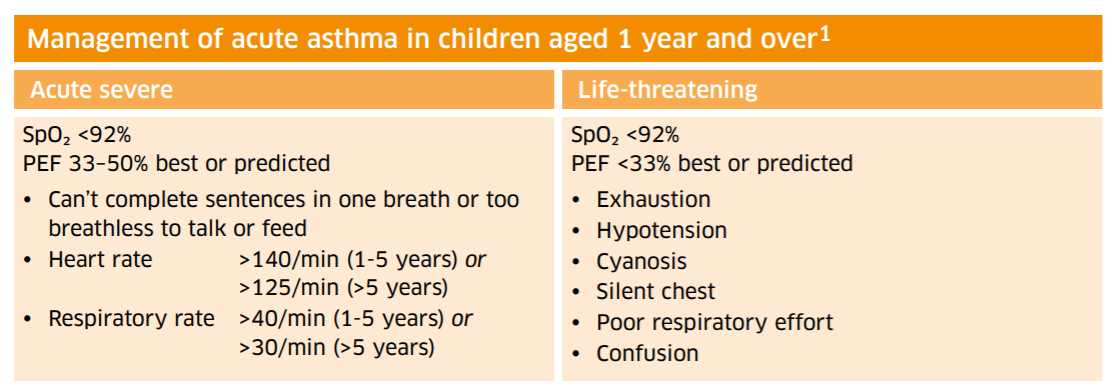
We noted that in reality in our ED the tannoy system is used to request urgent reviews. This has the potential to be impersonal “can a doctor come to…” and there is some risk of bystander effect with it. Do we assume someone else will go? Very early on the question of whether to move to resus was raised. To arrange this, one would need to speak to the team in Majors - when is a good time to leave the patient if this is what is needed? We discussed the usefulness of having a capillary blood gas if possible when discussing with the paediatric team. We discussed that the paediatric team may be far away, both in time and in space! So it’s important to highlight sick people to seniors within ED too, and keep treatment/monitoring going to make sure they’re still improving. In the feedback for the session it was raised whether doctors should rotate through allocated paediatric ED days. It was also asked about how to access asthma action plans - see the “to do” section below for this. The guideline: I can’t post the asthma guideline here but you can find it on the ED browser under children’s guidelines. It’s split into pdfs for each age range, and it’s a really straightforward single-page sheet. You can see how to grade the child’s observations into the severity of asthma attack, and there are clear treatment options. There is also an advice sheet for parents under the patient information leaflets section. Here is the BTS/SIGN equivalent in how to grade moderate vs severe vs life-threatening attacks (BTS/SIGN 2019) - the full guideline is under the “to do” section below. Key steps in child >5 years old:
To do: If it’s been a while since you worked in the paeds area, ask someone who is regularly there to show you where key items are [ ] The SIGN asthma guideline here [ ] Check out the asthma plans that can be downloaded from Asthma UK here [ ] If you took part in the sim, you can use this blog as a starter to reflect on your own experience of it [ ] See you at the next one! James Keitley - ED sim fellow -------------- References: British Thoracic Society and Scottish Intercollegiate Guidelines Network (2019). British guideline on the management of asthma: quick reference guide. Available from: https://www.brit-thoracic.org.uk/document-library/guidelines/asthma/btssign-asthma-guideline-quick-reference-guide-2016. Viewed 09/09/20. Photos either taken by the author or copyright- and attribution-free in the public domain. --------------- For clinical decisions please refer directly to appropriate guidance. This blog will not be updated.
3 Comments
Leave a Reply. |
Categories
All
The Derrifoam BlogWelcome to the Derrifoam blog - interesting pictures, numbers, pitfalls and learning points from the last few weeks. Qualityish CPD made quick and easy..... Archives
October 2022
|