|
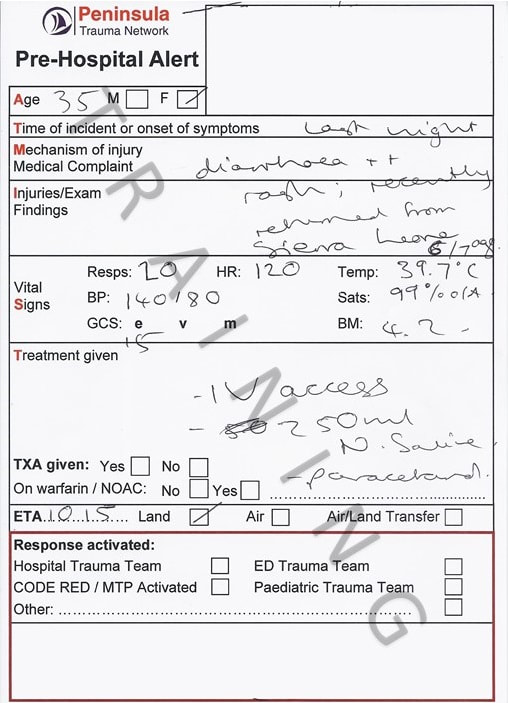
SimFridays sessions never seem to be on a Friday lately... so will be called "Sim ED" now instead! We did something a bit different and a bit scary in this one, and practised management of a patient with viral haemorrhagic fever (VHF). This tested our knowledge, team-working, and also the laboratory processes. The simulated case: Tanya is a woman in her thirties presenting with bloody diarrhoea, fever and a petechial rash. She returned 5 days ago from volunteering in Sierra Leone. What are the possible causes of this? Which of these are most common? Which are most serious? How would you approach a patient like this to cover the serious ones without overlooking common causes?
What did we think? In debrief we discussed: Horses vs zebras: From the outset of this simulation there was consideration of which diseases are endemic in the country the patient had visited, and VHF was considered likely. As a result one clinician reviewed alone in PPE and there were long discussions about tests, who to contact etc. It was pointed out that still common things are common and tasks like taking observations, giving fluids and antibiotics should not be delayed. Diagnoses like infectious gastroenteritis, sepsis, and even malaria are comparatively common so we need to both be wary of the serious but rare diagnosis whilst also cracking on with management of the more common options. Don’t forget the basics to avoid missing the horses! A really good A-E with attention to all vital signs and a brief history will help you act on the important horses question: IS THIS SEPSIS?... And treat it expeditiously. Explaining to the patient: Clearly coming to hospital in these circumstances would be very scary. I thought the patient explanations here were great and managed to explain the seriousness of the situation, gave clear instructions (“please do not leave the room”) whilst also being quite reassuring that the team had a good plan of what to do. Logistics of isolation and PPE: See the guidelines section below for what the SOP tells us about isolation for VHF. In this scenario the patient was isolated in a side room of majors. We discussed that a patient isolated like this must either have an en suite bathroom or at least a dedicated commode, and that this is very difficult to provide at present. We will be looking to source more. The patient’s blood sample labels were printed elsewhere by the runners and passed into the room to be applied to the samples. They were bagged once within the isolation room and dropped into a second bag held outside the room, before being put into a haze container and transported to the lab on foot. Clearly tasks like this require a good enough level of staffing to have people available nearby. The labs can send staff to collect the samples… don’t be afraid to ask for this when speaking to them.
Testing: The guidelines section below highlights specific requirements. In this scenario there were debate as to whether to delay taking blood until after the discussion with microbiology to ensure the correct samples were collected. Each time a sample is taken from a highly infectious patient there will be risk involved, so perhaps it is sensible if there is no immediate need, to confirm the tests first with the expert. We talked about how it has become automatic to process a venous blood gas for all patients. Because of splash risk it isn’t recommended in possible VHF cases, so perhaps one to think twice about how the results might change our management. Speaking to other teams: In the case of VHF there are many external people that need informing (see guidelines below). We talked about how long these discussions can take, and the importance of having concurrent tasks occurring that utilise different members of the team. Speaking up: We talked about team dynamics and the importance of speaking up and reminding the rest of the team of key actions. In this sort of rare presentation, it will be common to feel out of one’s depth and unsure, using your team to check any missed actions or specifically to read out the SOP is really helpful. As this blog has mentioned previously, closed loop communication (including use of first names) to confirm tasks, and graded assertiveness (see previous post on this) to remind others in the team, are both important. The guidelines: Probably the easiest place to find guidelines quickly for this patient is to go to the StaffNet homepage and use the search bar to find “viral fever” or “VHF”. The top option is an infection control page that talks about many diseases on different tabs, including VHF and Ebola. Alternatively there is a version inside the G drive under “Trust Documents”. I will highlight key parts here as a quick read. Please go to the source for the full info: Overview of VHF (info source Trust guidelines):
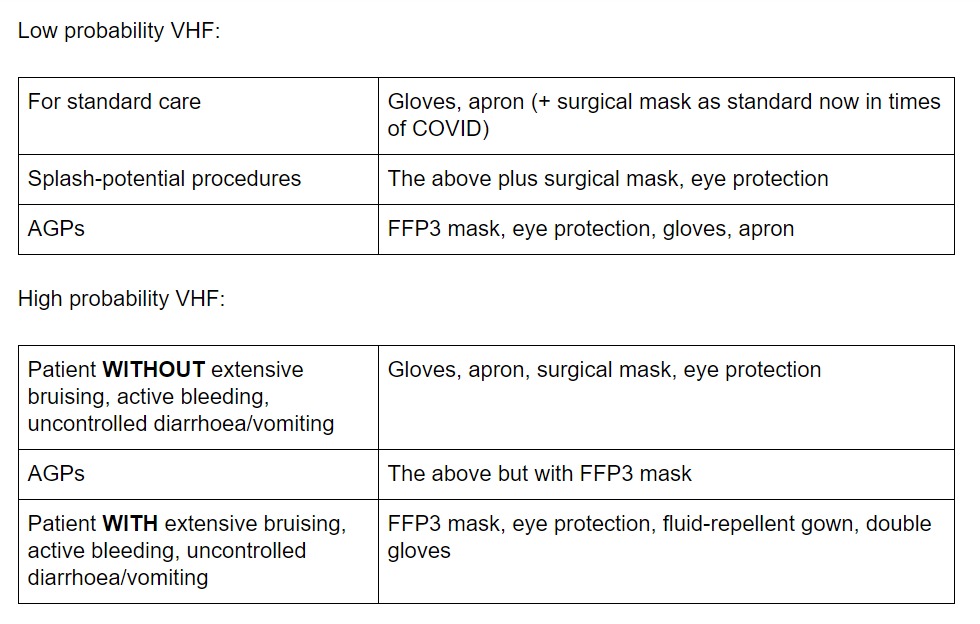
Triage assessment: If we know ahead that such a patient is coming, they should remain in the car park until cubicle 11 is ready for them to be transferred to directly. There is a VHF risk assessment flowchart on a single side of paper which you can easily follow to assess the likelihood of VHF. It also has brief but clear outcomes depending on the likelihood, and an overview of PPE required. This for me is the key part of the guidelines you must print for patients where it is being considered. There are negative-pressure isolation rooms in other departments, so ideally if VHF is considered likely from our flowchart the patient should be transferred to one of these via the bed manager or duty senior nurse, and then managed by the medical take team. Who to tell? Microbiology first. If thought to be likely VHF, switchboard can be asked to undertake the “critical internal incident call-out cascade” which will inform the necessary internal staff and open a major incident. The on-call director will then inform Public Health England and the other external agencies. Isolation and PPE: Side room with either en-suite bathroom or a dedicated commode. Ideally negative-pressure. The guidelines state exactly how to deal with laundry, spillages, waste etc. If the VHF screen comes back as positive the patient should be transferred to a HLIU (Royal Free London) and the local health protection team will be involved.
Testing: Urgent malaria testing (EDTA tube), FBC, U+Es, LFTs, clotting, CRP, glucose, blood cultures. Must call the combined labs ahead to inform them of the potential case. If high risk, they will send a haze container for the samples to be put inside. Must ask for a named contact in the lab to hand the sample to and provide a number to contact us back on. Must not use the pod system. The consultant microbiologist will organise the VHF screen from their side. The test is done on 1 x EDTA and 1 x clotted serum tubes. So, overall likely to need 3 x purple EDTA tubes, 2 x yellow serum tubes, 1 x blue and blood cultures. It is recommended generally not to use point-of-care blood gas testing due to splash-risk (Shorten and Wilson-Davies 2017). Management of contacts: If a patient has a “high probability” of VHF, a register must be kept of all staff entering the patient’s room (there is one ready to print in the guideline appendix). There are tables for how to manage contacts on pages 20 and 21 of the guidelines. Generally it involves self-monitoring temperature and reporting if symptoms develop. Interestingly, even for the highest risk contact (e.g. mucosal splash, needlestick, sexual contact) there are no restrictions on work or movements if asymptomatic, but they must monitor temperature and report to the monitoring officer daily. To do: Consider the next time you know ‘red PPE’ will be required for a case whether the donning/doffing guides in the PPE cupboard will be helpful to have nearby [ ] Have a look at the single-page risk assessment for VHF on StaffNet [ ] If you took part in the sim, you can use this blog as a starter to reflect on your own experience of it [ ] See you next time, James Keitley - ED Sim Fellow --------------- For clinical decisions please refer directly to the guidance. This blog may not be updated. All images copyright- and attribution-free in the public domain or taken by the author.
0 Comments
Leave a Reply. |
Categories
All
The Derrifoam BlogWelcome to the Derrifoam blog - interesting pictures, numbers, pitfalls and learning points from the last few weeks. Qualityish CPD made quick and easy..... Archives
October 2022
|