|
We were in ambulatory today thinking about the sort of patient that can slip under the radar. This was a patient with chest pain for whom aortic dissection was also a diagnostic possibility. The simulated case: A 66 year old man with hypertension, who has had sharp chest-through-to-back pain that started while out walking his dog. Think about cases where you have considered aortic dissection or seen it considered by other people - what are the aspects that raise it as a possibility? What happened?
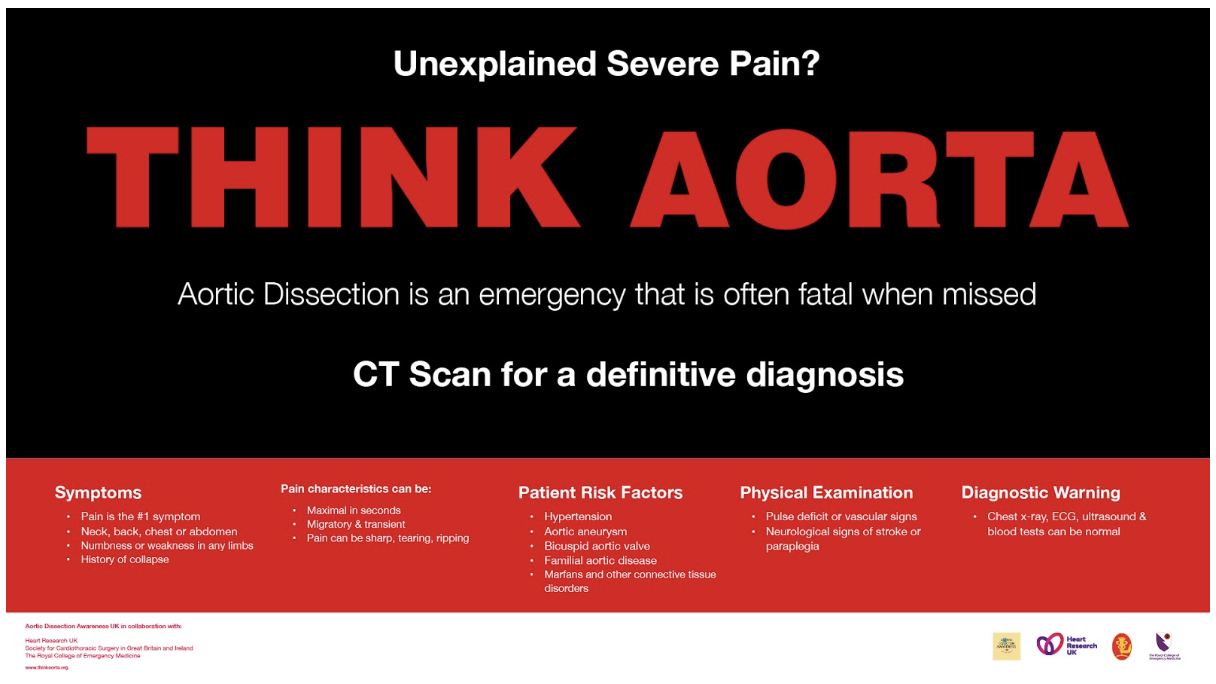
The patient had their blood taken in START, and was brought through into ambulatory for observations and an ECG. After a history and exam, aortic syndrome was considered more likely and they were transferred to majors while awaiting urgent CT angiogram. What did we think? In debrief we discussed: Threshold for considering the aorta: Aortic dissection can present in a variety of ways, and is often not the top diagnosis for the given presentation, so there needs to be a low threshold for considering it and looking for it. Although relatively uncommon, the high number of patients coming through ED means there could be around 1 per month in Derriford ED. Some resources refer to “chest pain plus one” where one looks for an additional feature alongside the chest pain that makes it atypical - e.g. back pain, abdominal pain, neurological changes. Mostly we are looking for:
There may be a pulse deficit or different BP in each arm, but these signs are not common and their absence does not exclude the diagnosis. In debrief we reviewed a chest x-ray with widened mediastinum, but again this is uncommon and a normal chest x-ray does not exclude aortic dissection. Logistics: The patient needed to move from ambulatory majors, for which the nurse in charge desk can be phoned to arrange. Patients would also need to move before they can have oxygen. They required an urgent CT angiogram, which also means a green cannula is needed. We thought about whether this patient might need an escort for the CT or not. Blood pressure management: The aortic dissection guideline on EDIS gives clear instructions regarding the management of blood pressure using labetalol. The target is a pulse of around 60 bpm and systolic BP under 110-120mmHg. If there is a discrepancy between arms the aim is to bring the higher result down, although one would need to be mindful not to drop the lower BP below the level required to perfuse. Closed loop communication: We talked about the use of closed-loop communication in this case to ensure tasks are being completed. The guidelines: The guideline is on EDIS under “adult medicine” and then “cardiology”. To do: Listen to “the aorta will #@&$! you up” (20 mins) online lecture here [ ] RCEM e-learning here [ ] If you took part in the sim, you can use this blog as a starter to reflect on your own experience of it [ ] James Keitley - ED Sim Fellow --------------- For clinical decisions please refer directly to the guidance. This blog may not be updated. All images copyright- and attribution-free in the public domain or taken by the author.
1 Comment
|
Categories
All
The Derrifoam BlogWelcome to the Derrifoam blog - interesting pictures, numbers, pitfalls and learning points from the last few weeks. Qualityish CPD made quick and easy..... Archives
October 2022
|