|
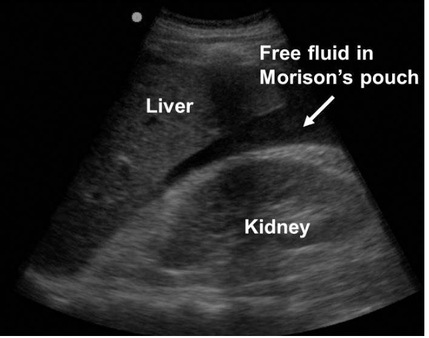
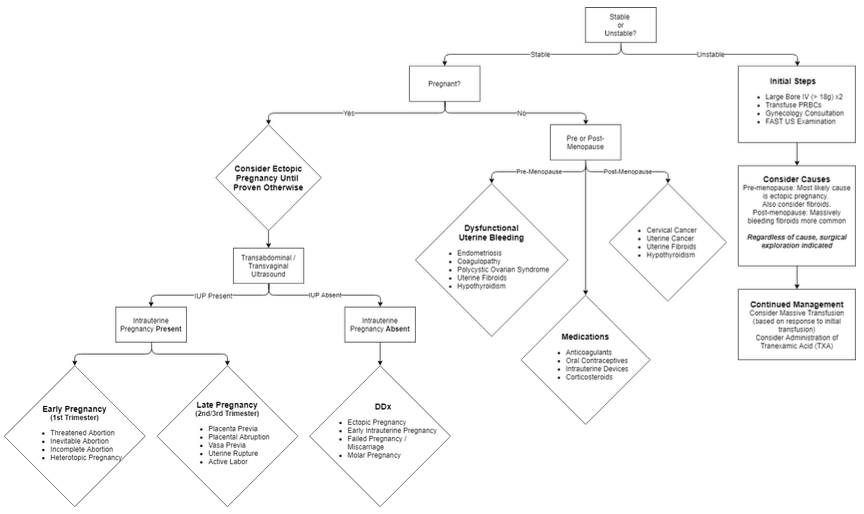
I was recently supposed to have been facilitating a session on vaginal bleeding as part of ACCS teaching so here is my attempt at a little bit of online education. Not my favourite subject on either a personal or professional level and don’t expect me to start speaking like a gynaecologist. A little Covid humour to start: Here goes. Everything an EM doctor needs to know on the glamorous topic of PV bleeding. Keep it simple, stupid: Question 1:Is the woman bleeding so heavily that they are showing signs of haemodynamic compromise? (Are they pale, ashen, sweaty? Peripherally shut down with a tachycardia? Hypotensive?). This is generally not a good sign and might make you feel a bit sweaty too. Take a deep breath, ask for some help and get the patient moved into resus. Take another deep breath and start reciting the alphabet: A and B – pop some oxygen on, C – if you have always wanted to insert a MASSIVE cannula then now is your chance. Two would be even better. Be kind if time allows and use a little local anaesthetic. Take some bloods and send some for an urgent cross-match. If the patient is really unwell then consider activating the massive transfusion protocol and starting a balanced transfusion (PRBC, FFP, platelets). Tranexamic acid is rarely a bad thing when people are bleeding a lot from any cause so think about it early. If you are a bit handy with the ultrasound or can find someone who is then it is worth scanning the abdomen for free fluid (has the patient ruptured an ectopic?). A gynaecologist is going to want to know about this patient sooner rather than later so get on the phone early. The most likely cause of shock due to vaginal bleeding is a ruptured ectopic pregnancy in a pre-menopausal woman and fibroids in a post-menopausal woman. Learning Bite: If the woman presents with signs of shock but with a BRADYCARDIA then you need to think about CERVICAL SHOCK. The patient will feel faint, sick and generally awful with hypotension and bradycardia. In the ED this is usually due to a miscarriage. It occurs when the products of conception pass through the cervix and cause a profound vagal response. The only treatment is to remove the products. This is a relatively simple procedure. The cervix is visualised with a speculum and the products are gently removed with sponge forceps (see below). It is very gratifying thing to do as the woman will literally improve before your eyes. One of our own registrars did this recently with good effect. It is important to think about it as a possibility and as always ask for help. Question 2: Is the woman pregnant? In Emergency medicine the dogma is that we should suspect pregnancy in any woman between the ages of 10 and 50. In reality most women know or recognise the possibility that they might be pregnant so do ask the question first. Establish when their last period was. Ask about symptoms of early pregnancy (e.g. breast tenderness, tiredness, urinary frequency). Try and get a urine sample as quickly as possible. If the pregnancy test is positive then the woman has a RUPTURED ECTOPIC until proven otherwise. Classically a ruptured pregnancy will present 6-8/52 after the woman’s last period. Pain is often more of a feature than bleeding. If the patient is unstable then they will be managed as described above. If the patient is stable then the bottom line is that they need a trans-vaginal ultrasound as soon as possible. This can happen as an in-patient or an outpatient depending on degree of suspicion, extent of symptoms and confidence that the patient will adhere to safety netting precautions if they are allowed home. Please discuss this with a senior and then refer to the gynae team. Make sure they have had the relevant bloods sent first – don’t forget a group and save in case they deteriorate and a serum beta-HCG is helpful as a baseline for the gynae team (they may monitor this serially). Clearly miscarriage is more common than an ectopic but is initially managed in the same way by us in the ED. PV bleeding in late pregnancy obviously has an entirely different differential including placental abruption, placenta previa, uterine rupture and labour. It is very rare to see such patients in our ED as they usually present to labour ward. If they do appear unexpectedly resuscitate as above and seek specialist help EARLY. Question 3: Is the woman pre or post-menopausal? Any woman with post-menopausal bleeding has cancer until proven otherwise. At the time of writing we don’t have access to the 2WW pathways so the patient will need a letter or phone call to their GP to get this sorted. We are now left with a pre-menopausal patient who isn’t haemodynamically compromised and isn’t pregnant. Breath. You now have time to take a bit more of a history! Questions that will help you elucidate what is going on:
So, what can we do in ED? (assuming as always that the patient is not in need of resuscitation)
References and Further Learning
1. NICE guidance on ectopic pregnancy and miscarriage: https://www.nice.org.uk/guidance/ng126 2. RCOG guidance on diagnosis and management of ectopic pregnancy: https://obgyn.onlinelibrary.wiley.com/doi/epdf/10.1111/1471-0528.14189 3. NICE guidance on heavy PV bleeding: https://www.nice.org.uk/guidance/ng88/resources/heavy-menstrual-bleeding-assessment-and-management-pdf-1837701412549 4. RCEM learning module on bleeding in pregnancy: https://www.rcemlearning.co.uk/modules/bleeding-in-pregnancy/
2 Comments
mike forster
25/6/2020 08:52:32
This is a very good run down. When the patient is stable and you need a early pregnancy scan you can call the EPU in daytime weekday or maternity reception out of hours and they will arrange.
Reply
Wendy James
25/6/2020 20:05:16
Love the light hearted humorous approach, made for very easy reading
Reply
Leave a Reply. |
Categories
All
The Derrifoam BlogWelcome to the Derrifoam blog - interesting pictures, numbers, pitfalls and learning points from the last few weeks. Qualityish CPD made quick and easy..... Archives
October 2022
|