|
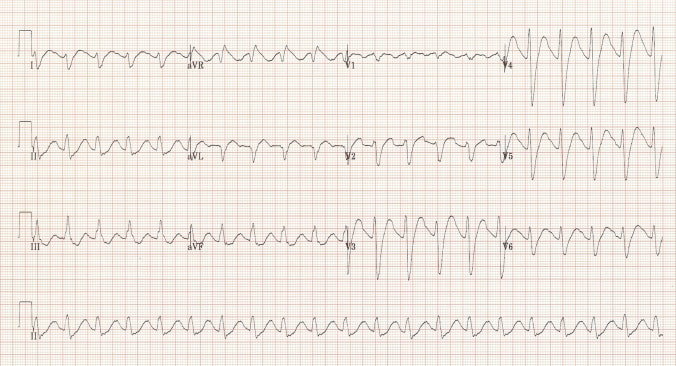
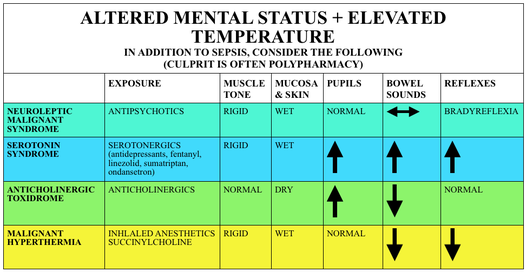
Case 33 year old male gradual onset of confusion, agitation distress; increasing over the past 6-12 hours recent GP visit for ? depression; question over possible recreational drug use (cannabis, ecstasy) On arrival in ED (RESUS) A- patent, protected B- RR 21/min; SpO2 98% OA ; clear chest C- hot to touch; HR 135 bpm; BP 160/100 mmHg D- agitated, restless, confused; pupils large (mydriasis) / Rigidity limbs, frequent myoclonic jerking movements / hyperreflexia; no meningism E- temp 38.2; no rash VBG - mild metabloic acidosis, lactate raised, glucose normal CXR normal ECG What is the differential diagnosis? What are the potential underlying causes? What is the treatment? Clinical Features of Serotonin Syndrome ‘CAN’ Central nervous system - AMS, seizures Autonomic dysfunction - HTN, hypotension, tachycardia, bradycardia, hyperthermia, dysrhythmias, flushing, sweating, mydriasis Neuromuscular dysfunction - rigidity LL>UL; hyperreflexia; clonus; tremor In practice, the diagnosis is often more of a gestalt impression based of the history, absence of other causes and the findings on physical examination. Potential underlying causes? Serotonergic agents either in overdose or a combination of therapeutic agents - Antodepressants: SSRIs & SNRIs (fluoxetine, citalopram, venlafaxine, duloxetine); TCAs; MAOIs - opioids (tramadol, pethidine, fentanyl, dextromethorphan) - antibiotics (linezolid) - antimemetics (metoclopramide, ondansetron) - mood stabilisers (lithium, sodium valproate) - recreational (amphetamines, ecstacy, LSD) - herbal (st john’s wart, ginseng) Treatment (RESUS-RSI-DEAD approach) RESUS - identify immediately life threats
- control ongoing seizures (BDZ; Phenytoin; intubation & ventilation) - correct hyperthermia
RISK ASSESSMENT
ANTIDOTES
Resources & further reading:
https://patient.info/doctor/serotonin-syndrome https://lifeinthefastlane.com/toxicology-conundrum-024/ http://www.emdocs.net/serotonin-syndrome-and-neuroleptic-malignant-syndrome-pearls-pitfalls/ http://www.emdocs.net/toxcard-differentiating-serotonin-syndrome-neuroleptic-malignant-syndrome/ https://emsimcases.com/2017/06/20/serotonin-syndrome/ http://foamcast.org/2015/05/04/episode-28-neuroleptic-malignant-syndrome-serotonin-syndrome-malignant-hyperthermia/ https://www.aliem.com/2012/01/paucis-verbis-serotonin-syndrome/ http://www.tamingthesru.com/blog/annals-of-b-pod/spring-2017/serotonin-syndrome
5 Comments
andy kelly
4/9/2017 13:36:37
NICE case - thanks
Reply
7/11/2018 06:40:37
Good information, thank u and please visit back my article~!
Reply
3/8/2022 15:29:17
Edirne Viessman servisi en uygun fiyat ve en hızlı servis garantisi ile sizlerle. https://www.edirneklimaservisi.com/edirne-viessmann-servisi/
Reply
Leave a Reply. |
Categories
All
The Derrifoam BlogWelcome to the Derrifoam blog - interesting pictures, numbers, pitfalls and learning points from the last few weeks. Qualityish CPD made quick and easy..... Archives
October 2022
|